Published 16 January 2024
Healing Beyond the Surface: Coping Strategies for Autoimmune Blisters
Understanding Autoimmune Blisters
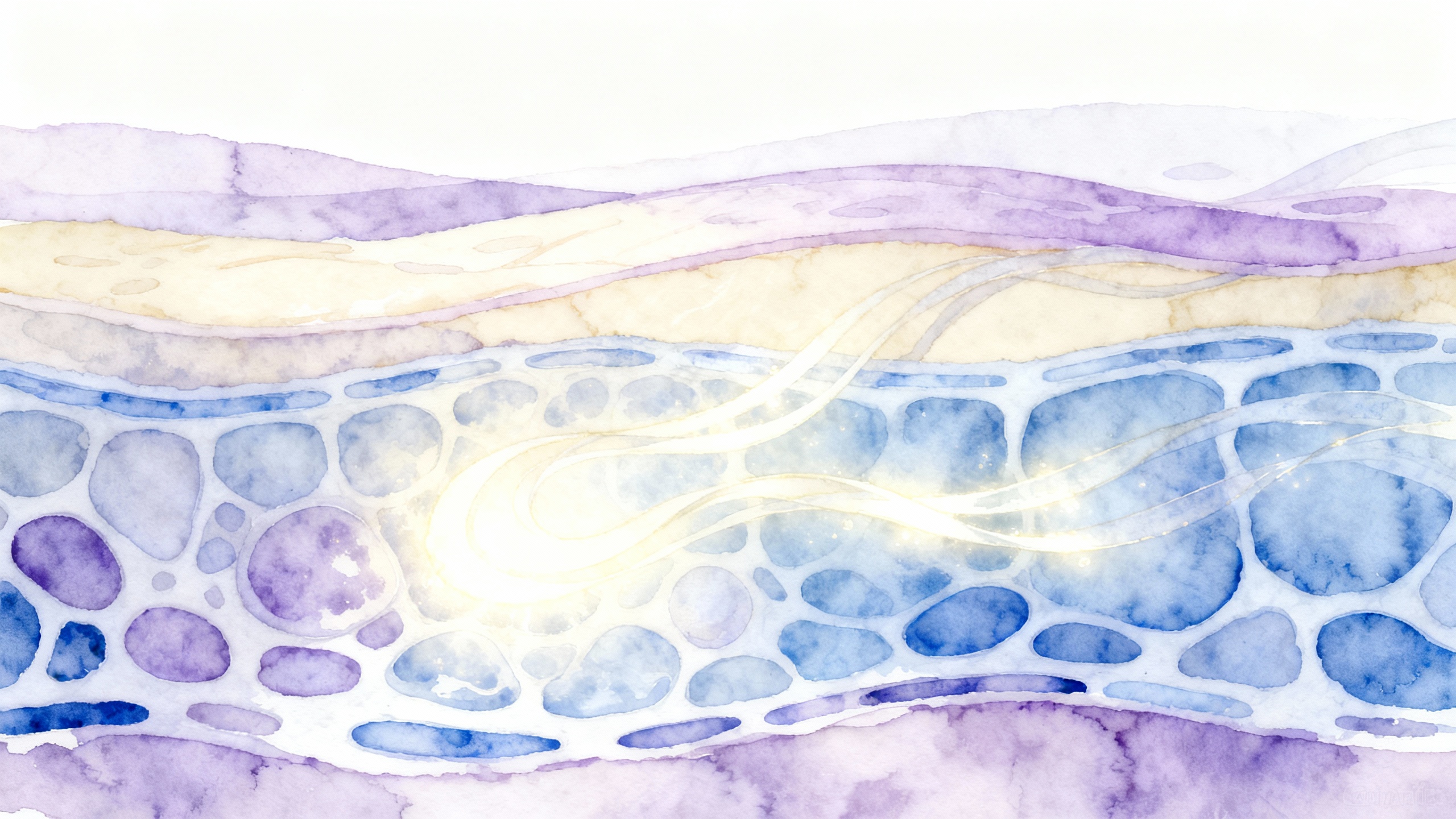
Autoimmune blisters are a challenging aspect of various autoimmune conditions that affect the skin. These blisters occur when the immune system mistakenly targets proteins within the skin, leading to the formation of painful and persistent blisters. Among the autoimmune blistering diseases, Pemphigus Vulgaris stands out as a commonly encountered condition.
What are Autoimmune Blisters?
Autoimmune blisters are characterized by the formation of fluid-filled blisters on the skin or mucous membranes. These blisters can be painful, itchy, and may rupture, leaving behind raw and sensitive skin. Autoimmune blistering diseases occur when the immune system mistakenly attacks proteins that are essential for maintaining the integrity of the skin and mucous membranes.
The exact cause of autoimmune blistering diseases is still unclear. However, factors such as genetic predisposition, environmental triggers, and certain medications may play a role in their development. It is important to consult with healthcare professionals for a proper diagnosis and appropriate management strategies.
Pemphigus Vulgaris: A Common Autoimmune Blistering Disease
Pemphigus Vulgaris is a chronic autoimmune blistering disease that primarily affects the skin and mucous membranes. It is characterized by the formation of fragile blisters that can easily rupture, leading to painful erosions. Pemphigus Vulgaris is caused by autoantibodies targeting desmoglein proteins, which are responsible for maintaining the integrity of skin cells.
This condition most commonly affects middle-aged and older adults, although it can occur at any age. The exact cause of Pemphigus Vulgaris is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Proper diagnosis and management of Pemphigus Vulgaris are essential to minimize symptoms and prevent complications.
To effectively cope with autoimmune blisters and manage the symptoms associated with conditions like Pemphigus Vulgaris, it is important to explore coping strategies, medical treatments, and seek support from healthcare professionals and support networks. In the following sections, we will delve into various coping strategies, lifestyle modifications, medical treatments, and the importance of seeking support for individuals with autoimmune blisters.
Coping Strategies for Autoimmune Blisters
Living with autoimmune blisters can be challenging, but there are strategies that can help you cope with the symptoms and reduce discomfort. Here are some coping strategies to consider:
Skin Care and Hygiene
Proper skin care and hygiene are essential for managing autoimmune blisters. Here are some tips to keep in mind:
- Gently cleanse the affected areas using mild, fragrance-free cleansers or non-soap cleansers.
- Avoid hot water and opt for lukewarm water when showering or bathing.
- Pat your skin dry instead of rubbing it with a towel to prevent further irritation.
- Apply moisturizers regularly to keep the skin hydrated and reduce dryness.
- Use non-adhesive dressings or bandages to protect the blisters and prevent friction.
- Consult with your healthcare professional or dermatologist for specific wound care instructions and recommendations.
For more information on wound care and preventing infections, refer to our article on wound care for pemphigus vulgaris blisters and preventing infections in pemphigus vulgaris blisters.
Pain Management Techniques
Managing pain associated with autoimmune blisters is crucial for improving your overall quality of life. Here are some techniques that may help:
- Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), may provide temporary relief. However, it’s important to consult with your healthcare professional before taking any medications.
- Topical pain relief creams or ointments containing lidocaine or capsaicin may help alleviate discomfort. These products should be used as directed and with caution.
- Cool compresses or ice packs applied to the affected areas can help numb the pain temporarily.
- Distraction techniques, such as deep breathing exercises, listening to music, or engaging in activities you enjoy, may help divert your focus away from the pain.
To learn more about managing pain from autoimmune blisters, you can refer to our article on managing pain from pemphigus vulgaris blisters.
Minimizing Skin Breakdown
To minimize skin breakdown and promote healing, consider the following tips:
- Avoid scratching or picking at the blisters, as this can lead to further damage and potential infections.
- Wear loose-fitting clothing made from soft, breathable fabrics to prevent friction and irritation.
- Protect the affected areas from the sun by using sunscreen with a high SPF, wearing protective clothing, or seeking shade.
- Maintain a healthy diet rich in nutrients, including vitamins and minerals that support skin health.
- Stay hydrated by drinking enough water throughout the day to keep your skin moisturized from within.
For additional self-care tips and lifestyle modifications for managing autoimmune blisters, refer to our article on self-care tips for pemphigus vulgaris.
By implementing these coping strategies and following a comprehensive treatment plan, you can improve your comfort level and minimize the impact of autoimmune blisters on your daily life. Remember to consult with your healthcare professional or dermatologist for personalized advice and guidance based on your specific condition.
Lifestyle Modifications
When dealing with autoimmune blisters, it’s essential to adopt certain lifestyle modifications that can help alleviate symptoms, prevent skin breakdown, and promote overall well-being. By making mindful choices in areas such as diet, stress management, and rest, individuals can effectively cope with the challenges posed by autoimmune blisters.
Dietary Considerations
Maintaining a healthy and balanced diet can play a significant role in managing autoimmune blisters. While there is no specific diet that can cure the condition, certain dietary considerations may help support overall skin health and reduce inflammation.
Including a variety of fruits, vegetables, whole grains, and lean proteins in your diet can provide essential nutrients and antioxidants that contribute to skin health. Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have anti-inflammatory properties that may help reduce inflammation associated with autoimmune blisters.
It’s also important to stay hydrated and drink an adequate amount of water throughout the day to keep your skin hydrated and promote skin elasticity. Avoiding excessive consumption of processed foods, refined sugars, and trans fats is advisable as they can potentially trigger inflammation and compromise skin health.
For more information on diet recommendations and potential foods to include or avoid, refer to our article on diet recommendations for pemphigus vulgaris.
Stress Management
Stress can exacerbate autoimmune blister symptoms and contribute to flare-ups. Therefore, incorporating stress management techniques into your daily routine is crucial for managing the condition effectively.
Practicing relaxation techniques, such as deep breathing exercises, meditation, and yoga, can help reduce stress levels and promote overall well-being. Engaging in hobbies, spending time with loved ones, and pursuing activities that bring joy and relaxation can also be beneficial in managing stress.
If you’re looking for more stress management techniques specifically tailored to pemphigus vulgaris, our article on stress management techniques for pemphigus vulgaris provides further guidance.
Importance of Rest and Sleep
Adequate rest and quality sleep are essential for individuals with autoimmune blisters. Fatigue and lack of sleep can worsen symptoms and compromise the immune system, making it harder for the body to heal.
Establishing a regular sleep routine, maintaining a comfortable sleep environment, and practicing good sleep hygiene can contribute to better sleep quality. It’s also important to prioritize rest and allow yourself time to relax and recharge.
If you’re experiencing difficulties with sleeping, our article on sleep strategies for pemphigus vulgaris sufferers offers valuable insights and techniques to promote better sleep.
By incorporating these lifestyle modifications, individuals with autoimmune blisters can enhance their overall well-being and better manage their symptoms. It’s important to remember that lifestyle modifications should be tailored to individual needs and preferences. Consulting with healthcare professionals and seeking support from peers and mental health professionals can provide further guidance and assistance in navigating the challenges of living with autoimmune blisters.
Medical Treatments for Autoimmune Blisters
When it comes to managing autoimmune blisters, medical treatments play a crucial role in providing relief and reducing blister formation. While these treatments may not cure the underlying autoimmune condition, they can help alleviate symptoms and improve quality of life. Here are three common medical treatments for autoimmune blisters:
Topical Medications
Topical medications are often the first line of defense when it comes to managing autoimmune blisters. These medications are applied directly to the affected skin and work to reduce inflammation, relieve pain, and promote healing. Common topical medications used for autoimmune blisters include:
- Topical corticosteroids: These anti-inflammatory medications help to reduce redness, swelling, and itching associated with blisters.
- Topical immunosuppressants: These medications work by suppressing the immune system’s response, helping to control blister formation and reduce inflammation.
- Topical antibiotics: In cases where blisters become infected, topical antibiotics may be prescribed to prevent further complications.
It’s important to follow the instructions provided by your healthcare professional when using topical medications. Proper application techniques and adherence to the prescribed treatment schedule are vital for effective management of autoimmune blisters. For more information on wound care and preventing infections, refer to our article on wound care for pemphigus vulgaris blisters and preventing infections in pemphigus vulgaris blisters.
Systemic Medications
In cases where topical medications alone are not sufficient, systemic medications may be prescribed to manage autoimmune blisters. These medications are taken orally or administered through injections and work to target the immune system as a whole. Common systemic medications used for autoimmune blisters include:
- Corticosteroids: These medications, taken orally or through injections, help to reduce inflammation and suppress the immune system’s response.
- Immunosuppressants: These medications work by modulating the immune system, preventing the production of antibodies that contribute to blister formation.
- Biologic therapies: These newer treatments target specific components of the immune system, providing more targeted and effective management of autoimmune blisters.
Systemic medications often require close monitoring and regular check-ups with healthcare professionals to assess their effectiveness and monitor potential side effects. It’s important to discuss any concerns or questions you have with your healthcare team to ensure the best possible outcome. For more information on managing symptoms and potential side effects of systemic medications, refer to our article on medications for pemphigus vulgaris relief.
Immunomodulatory Therapies
In addition to topical and systemic medications, immunomodulatory therapies may be considered for individuals with severe or refractory autoimmune blisters. These treatments aim to modify the immune response and can include:
- Intravenous immunoglobulin (IVIG): IVIG is a treatment where high doses of immunoglobulins, which are antibodies derived from donated blood, are administered intravenously. This therapy works to modulate the immune system and reduce blister formation.
- Plasmapheresis: Plasmapheresis involves removing a portion of the blood plasma, which contains the antibodies responsible for blister formation, and replacing it with donor plasma or a plasma substitute. This procedure helps to reduce the autoimmune response and alleviate blistering.
Immunomodulatory therapies are typically reserved for severe cases of autoimmune blisters and are administered under the supervision of trained healthcare professionals. It’s important to consult with your healthcare team to determine if these therapies are appropriate for your specific situation. For more information on long-term management and alternative therapies for autoimmune blisters, refer to our article on long-term management of pemphigus vulgaris symptoms and alternative therapies for pemphigus vulgaris.
Medical treatments for autoimmune blisters aim to provide relief, manage symptoms, and prevent complications. It’s important to work closely with your healthcare team to find the best treatment approach for your specific needs. Regular follow-ups and open communication with your healthcare professionals are essential for optimizing your treatment plan and achieving the best possible outcomes.
Seeking Support
Living with autoimmune blisters can be challenging, both physically and emotionally. It’s important to seek support and connect with others who may be going through similar experiences. Here are some strategies to consider for seeking support:
Support Groups and Online Communities
Joining support groups and online communities can provide a sense of belonging and understanding. Interacting with individuals who have firsthand experience with autoimmune blisters, such as pemphigus vulgaris, can offer invaluable support and knowledge. These groups often provide a safe space to share experiences, ask questions, and receive advice from others who truly understand the struggles and challenges associated with the condition. Additionally, participating in these communities can help alleviate feelings of isolation and provide a sense of empowerment.
Mental Health Support
Dealing with autoimmune blisters can take a toll on your mental well-being. It’s important to prioritize your mental health and seek professional support if needed. Mental health professionals, such as therapists or counselors, can provide guidance and coping strategies to help manage the emotional impact of living with chronic blistering diseases. They can offer a safe and non-judgmental space to express your feelings, develop effective coping mechanisms, and navigate the emotional challenges associated with the condition. Remember, seeking mental health support is just as important as seeking medical treatment.
Consulting with Healthcare Professionals
Never underestimate the importance of consulting with healthcare professionals when it comes to managing autoimmune blisters. Dermatologists and other medical specialists can provide essential medical guidance, monitor your condition, and recommend appropriate treatments and medications. They can also help you understand the underlying causes of blistering diseases and provide you with the necessary tools to manage symptoms effectively. Regular check-ups and open communication with your healthcare team are crucial for long-term management and overall well-being.
By seeking support through support groups, online communities, mental health professionals, and healthcare providers, you can find a network of understanding and guidance. Remember, you don’t have to face the challenges of autoimmune blisters alone. Seeking support can empower you to navigate the physical and emotional aspects of the condition, and ultimately, improve your overall quality of life.
